In today’s digital age, the healthcare industry is undergoing a transformative shift towards digitized processes and advanced technologies. Among these advancements, electronic medical records (EMR) software stands out as a cornerstone of modern healthcare data management. EMR software empowers healthcare providers to revolutionize the way patient information is stored, accessed, and shared. Gone are the days of cumbersome paper-based records that were prone to errors, difficult to access, and challenging to manage. EMR software replaces the traditional, manual record-keeping systems with a sophisticated digital infrastructure that offers seamless integration, enhanced security, and improved patient care. EMR software serves as a comprehensive and centralized repository for all patient-related information. It enables healthcare professionals to capture, organize, and retrieve critical patient data, including medical history, diagnoses, treatments, medications, lab results, and imaging reports. With EMR software, healthcare providers have instant access to accurate and up-to-date patient records, facilitating efficient care delivery and informed decision-making.
This transformative technology not only streamlines healthcare workflows but also facilitates collaboration among care teams. With EMR software, healthcare providers across different specialties and departments can easily access and contribute to a patient’s electronic medical record. This promotes continuity of care, eliminates redundancies, and enables seamless communication and care coordination. The importance of EMR software in modern healthcare cannot be overstated. Its impact spans across various aspects of healthcare delivery, including improved patient outcomes, enhanced operational efficiency, and optimized resource allocation. By harnessing the power of technology, EMR software empowers healthcare organizations to provide high-quality, patient-centered care in a secure and efficient manner.
In addition to its clinical benefits, EMR software also supports administrative functions within healthcare organizations. It automates tasks such as appointment scheduling, billing, and insurance processing, reducing paperwork, minimizing errors, and optimizing revenue management. By streamlining administrative processes, EMR software allows healthcare providers to focus more on patient care, enhancing overall operational efficiency. As the healthcare industry continues to evolve, so does the development of EMR software. Advancements in technologies such as artificial intelligence (AI), machine learning (ML), interoperability, and cloud computing are reshaping the landscape of EMR software. These innovations are unlocking new possibilities for data analytics, telemedicine integration, and patient engagement, further enhancing the capabilities and impact of EMR software.
The Importance of Electronic Medical Records (EMR) Software
EMR software holds immense importance in modern healthcare systems, driving improvements in patient care, operational efficiency, and data security. Here are key reasons why EMR software is crucial:
- Improved Accessibility: EMR software ensures that patient records are easily accessible to authorized healthcare providers, regardless of their physical location. This facilitates timely decision-making and seamless coordination of care among healthcare professionals.
- Enhanced Patient Care: EMR software enables comprehensive and up-to-date documentation of patient medical information, including medical history, diagnoses, treatments, medications, and allergies. This comprehensive view of patient data promotes continuity of care, reduces medical errors, and supports better treatment planning and personalized care delivery.
- Streamlined Workflow: By automating administrative tasks such as appointment scheduling, billing, and insurance processing, EMR software streamlines workflow processes. It eliminates paper-based inefficiencies, reduces redundant data entry, and empowers healthcare professionals to focus more on patient care.
- Secure Data Storage: EMR software provides secure data storage, protecting patient information from loss, damage, or unauthorized access. Robust security measures, including access controls, encryption, and audit trails, ensure compliance with data privacy regulations such as the Health Insurance Portability and Accountability Act (HIPAA).
- Interoperability and Information Exchange: EMR software facilitates seamless information exchange and interoperability between different healthcare systems, including hospitals, clinics, pharmacies, and laboratories. This promotes coordinated care, improves care transitions, and enhances collaboration among healthcare providers.
Key Features of Electronic Medical Records (EMR) Software
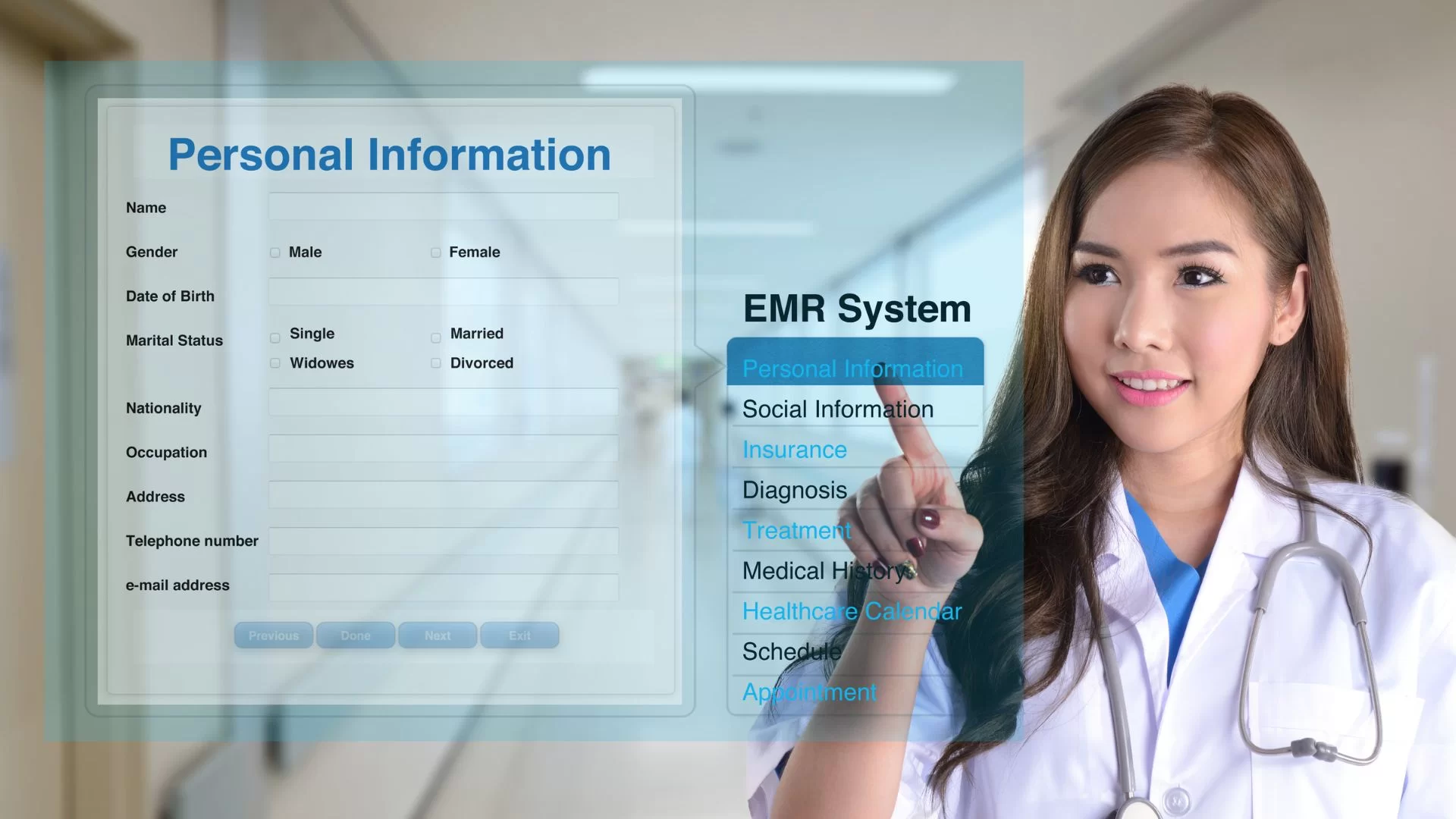
EMR software encompasses a range of features designed to effectively manage patient records and support healthcare workflows. Here are the key features of EMR software:
- Patient Records Management: EMR software enables the creation, storage, and retrieval of comprehensive patient records. It includes features for capturing patient demographics, medical history, allergies, medications, lab results, and imaging reports.
- Clinical Documentation: The software provides tools for healthcare professionals to document patient encounters, including progress notes, diagnoses, treatment plans, and procedures performed. It supports structured documentation and ensures accurate and consistent record-keeping.
- Electronic Prescribing: EMR software includes functionality for electronic prescribing (e-prescribing) of medications. It allows healthcare providers to generate and transmit electronic prescriptions directly to pharmacies, enhancing medication safety, reducing errors, and improving prescription trackingю
- Decision Support: EMR software can integrate clinical decision support tools that provide alerts, reminders, and evidence-based guidelines to assist healthcare professionals in making informed decisions. It helps ensure adherence to best practices, promotes patient safety, and supports clinical decision-making.
- Results and Imaging Management: The software enables the management and storage of laboratory test results, imaging reports, and other diagnostic data. It allows healthcare providers to efficiently review and track patient results, improving diagnostic accuracy and treatment planning.
- Interoperability: EMR software supports interoperability through standards such as Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR). It enables seamless data exchange and communication with other healthcare systems, promoting care coordination and ensuring the availability of critical patient information when needed.
- Appointment Scheduling: The software includes features for appointment scheduling, enabling healthcare providers to manage patient visits, assign time slots, and send automated reminders to patients. This ensures efficient utilization of resources, reduces no-show rates, and improves patient satisfaction.
- Billing and Coding Integration: EMR software can integrate with billing and coding systems, automating the billing process and ensuring accurate coding for services rendered. This integration improves revenue management, reduces administrative burden, and enhances financial efficiency for healthcare organizations.
- Security and Privacy: EMR software incorporates robust security measures to protect patient data. It includes access controls, encryption, audit trails, and compliance with data privacy regulations such as HIPAA. These security measures ensure confidentiality, integrity, and availability of patient information.
Electronic Medical Records (EMR) Software Development Process
Developing EMR software requires a systematic approach to ensure its successful creation and implementation. Here are the key stages of the EMR software development process:
- Requirement Gathering: This initial stage involves conducting in-depth discussions with healthcare providers, administrators, and other stakeholders to gather requirements. The focus is on understanding their specific needs, workflows, and desired functionalities in the EMR software.
- System Design and Planning: Based on the requirements gathered, a detailed system design and architecture are created. This includes defining the database structure, user interfaces, and system modules. Planning the technical infrastructure, including servers, networks, and storage, is also done in this stage.
- Software Development: The development phase involves writing code and building the EMR software. It includes creating the database schema, implementing user interfaces, developing modules for patient records management, clinical documentation, prescribing, decision support, and other identified features. The software development follows best practices, coding standards, and utilizes appropriate programming languages and frameworks.
- Testing and Quality Assurance: Rigorous testing is performed to ensure the EMR software functions as intended, is free from bugs and errors, and meets the specified requirements. This includes functional testing, performance testing, security testing, and user acceptance testing. Any issues identified during testing are addressed and fixed.
- Deployment and Training: Once the software passes testing, it is deployed in the healthcare organization’s environment. This involves installing the software, configuring it based on the organization’s needs, and integrating it with existing systems. Training programs are conducted to familiarize healthcare professionals and staff with the software’s functionalities and ensure its effective use.
- Maintenance and Support: After deployment, ongoing maintenance and support are provided to ensure the EMR software operates smoothly. This includes regular updates to address bugs, security patches, and compatibility with new technologies. Technical support is offered to assist users with any questions or issues they encounter, ensuring continuous system availability and performance.
Future Trends in Electronic Medical Records (EMR) Software
EMR software continues to evolve to meet the changing needs of the healthcare industry. Here are some future trends that are shaping the development of EMR software:
- Cloud-Based Solutions: Cloud-based EMR solutions are gaining popularity due to their scalability, accessibility, and cost-effectiveness. Cloud platforms offer secure data storage, easy data sharing, and seamless collaboration among healthcare providers.
- Mobile Applications: Mobile applications are being developed to provide access to EMR software on smartphones and tablets. Mobile EMR apps allow healthcare professionals to access patient information, update records, and communicate with colleagues while on the go, improving efficiency and care coordination.
- Artificial Intelligence (AI) and Machine Learning (ML): AI and ML technologies are being integrated into EMR software to automate tasks, improve decision-making, and enhance patient care. AI-powered algorithms can analyze patient data, detect patterns, predict outcomes, and assist healthcare professionals in making accurate diagnoses and treatment plans.
- Patient Engagement Features: EMR software is incorporating patient engagement features to empower patients in their healthcare journey. This includes patient portals, online appointment scheduling, secure messaging with healthcare providers, access to lab results, and educational resources. Engaging patients in their care improves patient satisfaction and outcomes.
- Voice Recognition and Natural Language Processing: Voice recognition and natural language processing technologies are being integrated into EMR software to enable voice-based documentation, making it more efficient and reducing the time spent on manual data entry. These advancements enhance usability and workflow efficiency.
- Blockchain Technology: Blockchain technology is being explored for its potential to enhance data security, privacy, and interoperability in EMR software. It offers decentralized and tamper-proof data storage, ensuring data integrity, secure patient consent management, and seamless data exchange among authorized parties.
As EMR software continues to evolve, it will play a crucial role in digitizing healthcare organizations and improving patient care. By embracing these future trends, healthcare providers can leverage technology to streamline workflows, enhance communication, and deliver better outcomes for patients.
Integration with Medical Devices and IoT
The Integration with Medical Devices and IoT section focuses on the significance of integrating Electronic Medical Records (EMR) software with medical devices and Internet of Things (IoT) technologies. This integration enhances data capture, improves patient monitoring, enables real-time data analysis, and facilitates comprehensive healthcare management.
Integrating EMR software with medical devices and IoT technologies enables automatic and seamless data capture from various devices used in patient care. This includes devices such as vital sign monitors, wearable sensors, infusion pumps, and imaging equipment. By integrating these devices with the EMR software, patient data, measurements, and readings can be directly and accurately recorded in real-time, eliminating manual data entry and reducing the risk of errors.
One of the key advantages of this integration is improved patient monitoring and care. Real-time data from medical devices can be continuously transmitted to the EMR software, providing healthcare providers with immediate access to critical patient information. This enables timely intervention, early detection of abnormalities, and proactive management of patient conditions, ultimately leading to improved patient outcomes.
The integration also enables comprehensive data analysis and decision support. By capturing data from medical devices, the EMR software can perform real-time analytics and generate actionable insights. This allows healthcare providers to identify trends, monitor treatment effectiveness, and make data-driven decisions regarding patient care. The integration with IoT technologies further expands the possibilities, as data from various sources can be aggregated and analyzed, providing a holistic view of the patient’s health status.
Furthermore, the integration with medical devices and IoT technologies enhances workflow efficiency. Patient data is automatically recorded and readily available within the EMR software, eliminating the need for manual data entry and reducing administrative burdens. This enables healthcare providers to focus more on patient care, streamline processes, and improve overall productivity.
In addition, integrating EMR software with medical devices and IoT technologies promotes patient engagement and empowerment. With wearable devices and IoT-enabled home monitoring systems, patients can actively participate in their own healthcare management. Real-time data from these devices can be integrated into the EMR software, allowing patients and healthcare providers to track progress, monitor treatment adherence, and collaborate more effectively in managing chronic conditions or post-operative care.
However, it is crucial to address challenges related to data interoperability, standardization, and privacy when integrating EMR software with medical devices and IoT technologies. Ensuring secure data transmission, adhering to regulatory requirements, and maintaining patient privacy are critical considerations.
Mobile and Remote Access
The Mobile and Remote Access section highlights the importance of incorporating mobile and remote access capabilities in Electronic Medical Records (EMR) software. This integration enables healthcare providers to access patient information and clinical data from mobile devices or remote locations, enhancing care coordination, improving efficiency, and facilitating patient engagement.
Mobile access allows healthcare providers to securely access EMR systems through smartphones, tablets, or other portable devices. This mobility empowers clinicians to access patient records, review test results, update documentation, and make informed decisions at the point of care, regardless of their physical location. By eliminating the need for providers to be tethered to a fixed workstation, mobile access enhances workflow efficiency and reduces the potential for delays or errors in care delivery.
Remote access capabilities extend the benefits of mobile access by allowing healthcare providers to securely access EMR systems from remote locations outside of the healthcare facility. This feature is particularly valuable for telemedicine, home healthcare, or healthcare providers on-the-go, as it enables them to retrieve patient data, document encounters, and communicate with colleagues seamlessly. Remote access ensures continuity of care and enables timely decision-making, even when providers are not physically present in the clinic or hospital.
The integration of mobile and remote access in EMR software also facilitates care coordination and collaboration among healthcare teams. With real-time access to patient records and clinical data, providers can easily communicate and share information with colleagues, specialists, or consultants, regardless of their location. This improves care coordination, enables faster consultation, and enhances interdisciplinary collaboration, ultimately benefiting patient outcomes.
Furthermore, mobile and remote access capabilities promote patient engagement and empowerment. Patients can securely access their own health records, review lab results, request prescription refills, or communicate with their healthcare providers through secure patient portals or mobile applications. This fosters active participation in their own care, enhances communication, and supports shared decision-making between patients and providers.
From a practical standpoint, mobile and remote access can also contribute to cost savings and operational efficiencies. Providers can document encounters, order tests, or prescribe medications remotely, reducing the need for paper-based processes and streamlining administrative tasks. Additionally, remote access can facilitate remote monitoring of patients with chronic conditions, reducing hospital readmissions and improving overall healthcare resource utilization.
It is important to note that security and privacy considerations are of utmost importance when implementing mobile and remote access in EMR software. Robust security measures, such as encryption, authentication, and secure network protocols, must be in place to protect patient data and ensure compliance with privacy regulations.
Interoperability and Health Information Exchange
The Interoperability and Health Information Exchange section emphasizes the critical role of seamless data sharing and communication between healthcare systems and providers. Interoperability enables the exchange of patient information, such as medical records, test results, and treatment plans, in a standardized and secure manner. This exchange enhances care coordination, improves patient safety, and fosters informed decision-making.
Interoperability ensures that different healthcare systems, such as Electronic Health Records (EHR) systems, laboratory systems, pharmacy systems, and imaging systems, can effectively communicate and share data with each other. By adhering to standardized data formats and protocols, interoperable systems overcome the barriers of disparate data silos, allowing for comprehensive and holistic patient information.
The exchange of health information plays a crucial role in facilitating continuity of care. When patients seek care from different providers or transition between healthcare settings, their medical information needs to be readily available. Interoperability enables the seamless transfer of patient data, ensuring that healthcare providers have access to the most up-to-date and relevant information. This promotes accurate diagnosis, appropriate treatment planning, and avoids unnecessary duplication of tests or procedures.
Interoperability also improves care coordination among different healthcare providers involved in a patient’s care journey. When multiple providers can access and contribute to a shared patient record, it fosters collaboration, reduces miscommunication, and enables better coordination of treatment plans. This is particularly valuable in cases of complex or chronic conditions that require a multidisciplinary approach.
Moreover, interoperability enhances patient safety by reducing the risk of errors, adverse events, and medication mismanagement. Access to complete and accurate patient information allows healthcare providers to make informed decisions, verify medication allergies, identify potential drug interactions, and avoid duplicate or conflicting treatments. This leads to safer and more effective care delivery.
Interoperability also paves the way for data-driven healthcare initiatives, research, and population health management. Aggregated and anonymized data can be utilized for population health analysis, epidemiological studies, and clinical research. Interoperability enables the pooling of data from different sources, providing valuable insights into disease patterns, treatment outcomes, and healthcare trends.
However, achieving seamless interoperability and health information exchange faces challenges related to technical standards, data privacy, and governance. The adoption of standardized data formats, such as HL7 FHIR, and the implementation of robust privacy and security measures are essential for successful interoperability.
In conclusion, electronic medical records (EMR) software is transforming healthcare data management by enabling secure storage, efficient access, and seamless exchange of patient information. With its key features and continuous evolution driven by future trends, EMR software empowers healthcare providers to deliver high-quality care, improve patient outcomes, and drive operational efficiency. Embracing EMR software development is crucial for healthcare organizations to adapt to the digital age and provide better patient-centric care.